Dry eye syndrome is a disorder of the tear film due to tear deficiency, or excessive evaporation, which may cause damage to the ocular surface and is associated with symptoms of ocular discomfort. It is often accompanied with increased osmolarity and inflammation of the ocular surface. Usual symptoms include grittiness, irritation, blurred vision, foreign body sensation, glare sensitivity, burning, itchiness, and sometimes excessive tearing due to lacrimal glands over secretion by way of compensation.
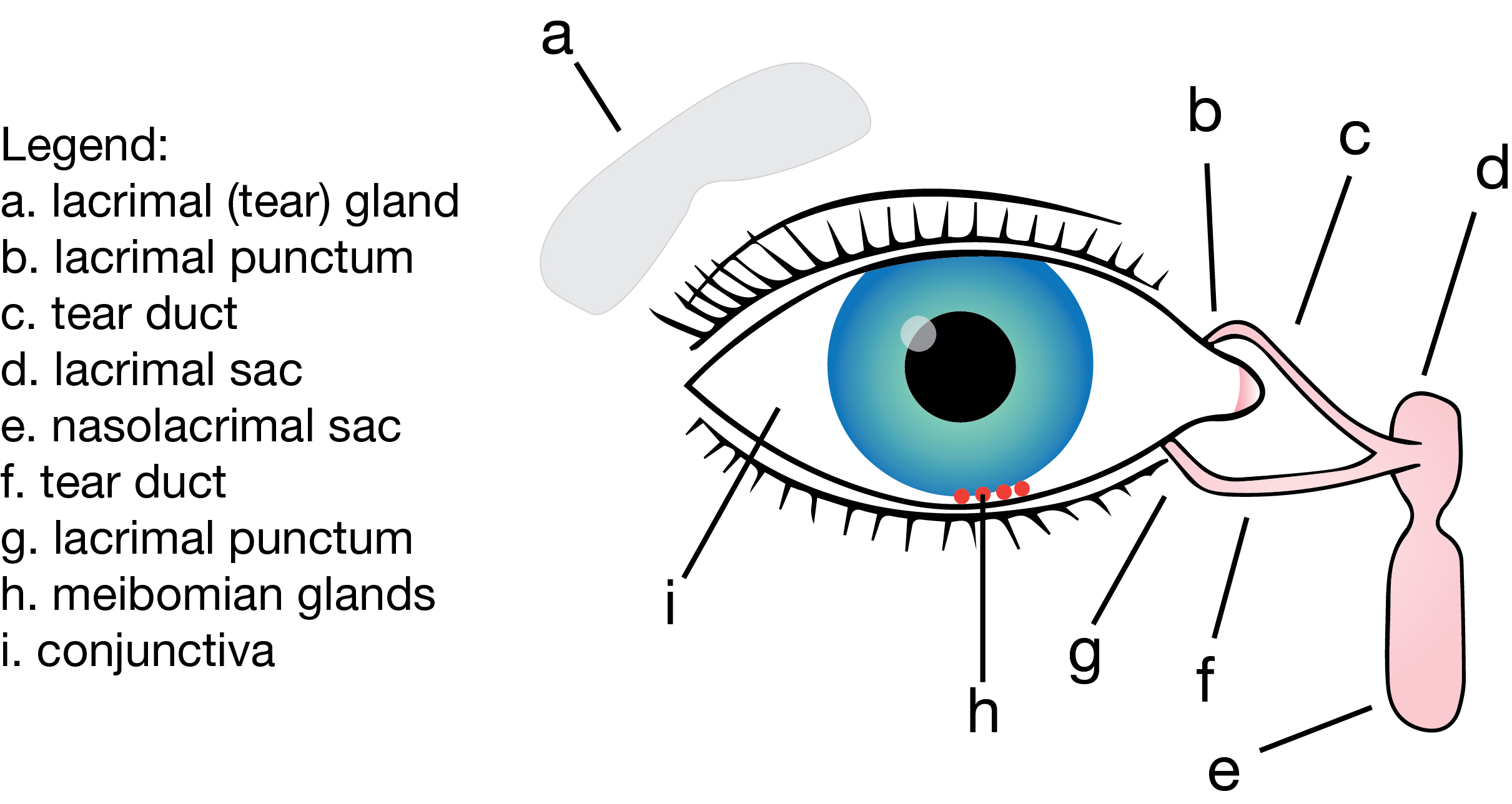
The normal tear film contains three layers which are a mucus layer, an aqueous layer and a lipid layer. The mucus layer is located closest to the cornea and is formed by the goblet cells found in the conjunctiva. It coats the eye and enables adherence of the tear film to the eye. The aqueous layer sits on top of the mucus layer and is formed by the lacrimal (tear) gland located above the eye socket. It is composed primarily of saline and electrolytes, and brings moisture and oxygen to the cornea. The lipid layer is the top layer and is formed by the meibomian glands.
The average eye has approximately 20 to 25 meibomian glands per eyelid and dry eyes usually result when they get blocked or destroyed because the primary function of the lipid layer is to prevent evaporation of the aqueous layer.
This is also the reason why most tear drops only temporarily relieve dry eyes because they only replenish the aqueous layer and in the process wash away the lipid layer, thereby disrupting the tear film.
Figure 1. Tear system. Adapted with permission from User: FML and Erin Silversmith.
Causes of Dry Eyes
- Age – due to the slowdown in the productivity of the glands
- Autoimmune diseases like Sjörgren’s syndrome, and autoimmune connective tissue diseases such as rheumatoid arthritis and lupus erythematosus, will often decrease the quantity of tears that are produced due to the chronic inflammation of the lacrimal gland associated with these diseases
- Excessive computer use which increases eye strain and reduces the eye blinking reflex (by up to 30%) leading to increased evaporation of the aqueous layer
- Triggers that can cause lacrimal gland inflammation may include contact lenses, contact lens cleaning solutions, preserved eye drops, eye infections, allergies, and even some vitamin deficiencies. It is important to note that the preservatives in eye drops tend to be toxic and irritant to the eye cells in the same way that they are toxic to bacterial cells
- Environmental factors such as air conditioning with dehumidifiers which encourage evaporation of the aqueous layer
- Medicines especially anticholinergics, diuretics, antihistamines, decongestants, pain medication (opioids), dermatological preparations (Roaccutane®), proton pump inhibitors, and H2 receptor antagonists, and
- Hormones whereby oestrogens cause dry eyes and androgens reduce dry eyes, hence women are more prone to dry eyes.
Treatment of Dry Eyes
First Line
- Education on the importance of blinking. Blinking exercises should be introduced, especially to people working with computers
- Modifying the environment, for example using air conditioners with humidifiers
- Nutritional support to increase food with omega-3 fish oil and salmon to ensure integrity of the tear film, and
- Review any medications and allergies which the patient might have that contribute to dry eyes.
Second Line
- Using unpreserved lubricating eye drops. This is more important than the choice of lubricant as there is no evidence that any lubricant is more superior to another
- Gels and nighttime ointments (especially for patients who sleep with their eyes open), and
- Use of topical steroids and topical cyclosporin.
Third Line
- Oral tetracyclines, and
- Punctal plugs inserted into the tear ducts, or puncta, to prevent tear drainage once any inflammation present is controlled.
Fourth Line
- Systemic immunosuppressants
- Moisture goggles and use of devices such as the Lipiflow®, and
- Punctal surgery to cut drainage completely.
A novel treatment is to use mist sprays such as Tearsagain®, which contain lecithin, and is sprayed directly onto a closed eye (simple administration) while not affecting any makeup or contact lenses. The mist spray stabilises the lipid layer and adds to the aqueous layer.
Tearsagain® is longer lasting (up to four hours) and can be used 3-4 times daily. It also does not contain preservative and is sterile for up to six months. It, however, relies on the blinking reflex for distribution hence is not effective while the patient is asleep and gel or ointments might be required for nocturnal symptoms.
References:
- Kokkinakis J. Dry Eyes [course notes]. Proceedings of the NSW Pharmacy – National Convention and Exhibition; 2013 June 21-23; Sydney, New South Wales.
- Rossi S ed. Australian Medicine Handbook 2013. Adelaide: Australian Medicines
Handbook Pty Ltd; 2013.
