Potassium is the primary intracellular cation in the blood. Most intracellular potassium is contained within muscle cells. Together with sodium it plays a role in maintaining osmotic balance. The ratio between intracellular and extracellular potassium concentration influences cell membrane polarisation, which in turn influences important cell processes, such as nerve impulses and muscle cell (including myocardial) contraction. Potassium is also involved in acid-base balance.
The normal physiological value of plasma potassium is 3.4-4.5mmol/L and serum potassium is 3.8-4.9mmol/L. Serum potassium is higher than plasma as a result of contamination by intracellular red blood cell potassium.
Hyperkalaemia
Hyperkalaemia occurs when serum or plasma potassium exceeds 5mmol/L. Hyperkalaemia is usually asymptomatic until cardiotoxicity occurs. Signs and symptoms of hyperkalaemia are muscle weakness and abnormalities of cardiac conduction.
The most common cause of hyperkalaemia is chronic renal disease, where renal potassium excretion is diminished. Additionally, hyperkalaemia occurs when there is transcellular movement of potassium out of cells, such as in the case of metabolic acidosis.
Insulin is responsible for moving potassium into cells hence hyperglycaemia, and in the presence of insulin deficiency, causes potassium to move out of cells. This raises plasma potassium.
When muscle fibre breaks down in rhabdomyolysis, potassium leaks out from muscle cells and causes an increase in plasma potassium.
Drugs can also increase plasma potassium. Examples are: potassium sparing medication (spironolactone, amiloride, triamterene), potassium supplements (including glucosamine potassium chloride complex), angiotensin converting enzyme inhibitors (perindopril, ramipril), trimethoprim, non-steroidal anti-inflammatories, digoxin toxicity, and suxamethonium.
The risk of hyperkalaemia increases when these medicines are used together, especially when combined with potassium supplements. If potassium is supplemented intentionally, serum potassium and renal function should be monitored to manage the risk.
Treatment of hyperkalaemia depends on the clinical context and degree of urgency. Electrocardiograph (ECG) is often used to assess the degree of urgency. For example, if there are ECG changes, ventricular arrest is likely, and hence is considered urgent. ECG changes occur when serum potassium is more than 5.5 mmol/L.
Initial changes in ECG (Figure 1) are shortening of the QT interval and tall, peaked T waves.
Figure 1. ECG patterns in hyperkalaemia.
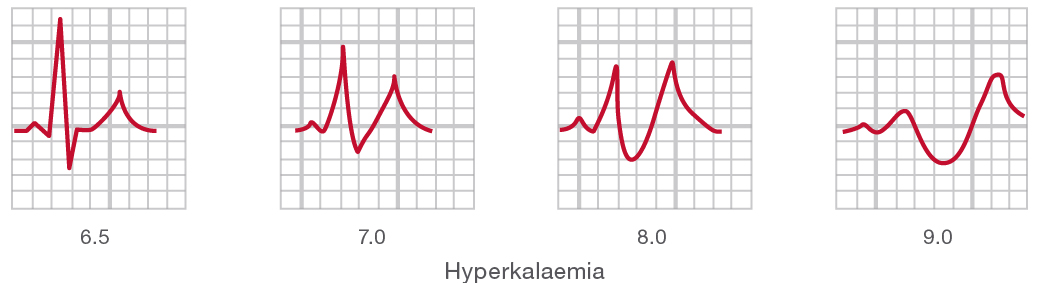
As serum potassium increases further, there is widening of the QRS complex, PR interval prolongation and disappearance of the P wave. Finally, the QRS complex degenerates into a sine wave pattern resulting in ventricular fibrillation.
Emergency treatment for hyperkalaemia is calcium gluconate 10% 10ml, given intravenously over two to three minutes into a large vein with ECG monitoring of the response. The response is immediate but not long lasting. The dose should be repeated if symptoms recur. Calcium works by antagonising the effect of hyperkalaemia on cardiac muscle excitability, but does not lower serum potassium. Intravenous glucose and insulin are usually given next, to promote cellular uptake of potassium. Short acting insulin (ten units) is usually given as an intravenous bolus, along with glucose 50% 50ml over five minutes. Glucose is not given if the patient is hyperglycaemic.
If metabolic acidosis is present, intravenous sodium bicarbonate 8.4% 50ml is given over 5-10 minutes under ECG control. This may be repeated in 60-120 minutes.
Salbutamol may be given intravenously or via nebuliser to stimulate the sympathetic nervous system and help shift potassium into cells. Frusemide is also used to increase potassium excretion, provided the patient is not renally impaired.
Potassium can be removed from the bowel lumen in exchange for sodium, by administering sodium polystyrene sulfonate 15g orally (suspended in 50-100mL of water), three to four times daily. Onset of action is slow (1-2 hours), hence it should not be used first-line in an emergency situation. Electrolyte disturbances are common and electrolytes should be monitored regularly while undergoing treatment. Side effects like constipation can be managed with laxatives. It should be noted that laxatives containing sorbitol should be avoided due to the risk of colonic necrosis.
Finally, haemodialysis can be performed in patients with renal failure or if emergency treatment is ineffective.
Hypokalaemia
Hypokalaemia is when the level of serum potassium is less than 3mmol/L. The main clinical features of hypokalaemia are: impaired muscle function (i.e. weakness, muscle fatigue, cramps and myalgias) and cardiovascular symptoms (hypertension and cardiac arrhythmias).
Cardiovascular symptoms occur when the serum potassium is less then 3mmol/L.
The ECG patterns in hypokalaemia (Figure 2) show initial sagging of the ST segment, depression of the T wave and elevation of the U wave. As serum potassium decreases further, the T wave becomes inverted or increasingly smaller and the U wave becomes larger.
Figure 2. ECG patterns in hypokalaemia.
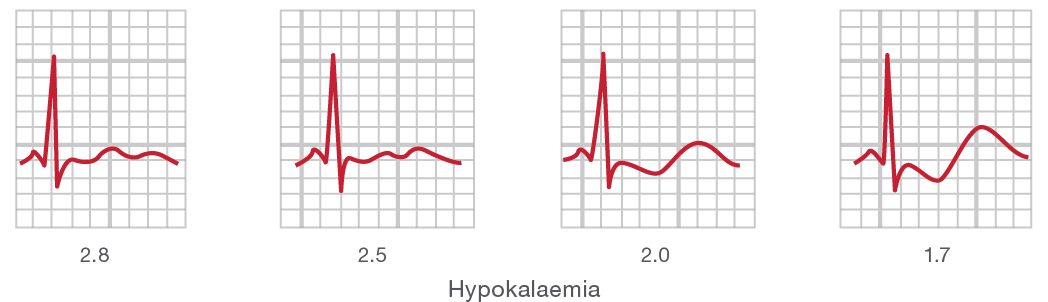
The consequences are ventricular and atrial tachyarrhythmias, and second or third degree atrioventricular block.
Causes of hypokalaemia are usually due to losses from the kidneys or the gastrointestinal tract (vomiting and diarrhoea).
Drugs like diuretics cause hypokalaemia by enhancing renal excretion. Other drugs with similar effects are high dose penicillins (ampicillin, penicillin), mineralocorticoids, aminoglycosides, amphotericin B and cisplatin.
Some drugs cause hypokalaemia by shifting potassium into cells. Examples are: insulin, beta 2 agonists such as terbutaline, caffeine and theophylline.
Identifying the route and cause of the loss of potassium is important in determining the treatment for hypokalaemia. When hypokalaemia is persistent and unresponsive to treatment, continuing loss could indicate the possibility of anorexia, acid-base disturbances, magnesium deficiency, or diuretics and laxatives being abused as weight loss agents.
Replacement can be initiated with oral potassium chloride (KCl) supplementation at a dose of 1200-3600mg daily. Potassium can cause gastric irritation and sometimes bleeding, hence it is recommended to be taken with food, in divided doses. Liquid KCl is effective in increasing levels within two hours, however is poorly tolerated due to its bitter taste.
The parenteral form is given in severe cases, where muscle paralysis is present or where cardiac rhythm disturbance relates to hypokalaemia. The dose of intravenous potassium chloride is 30mmol/L given over 3-12 hours. Potassium concentration should not exceed 40mmol/L and the rate of potassium infusion should not exceed 10mmol/hour to avoid potential heart block and fatal hyperkalaemia.
In the emergency treatment of diabetic ketoacidosis or hypokalaemia induced arrhythmia, the rate of infusion could be increased, however caution should be taken to monitor potassium concentration, ECG, and fluid balance regularly. Intravenous potassium is given in saline containing solution rather than dextrose, as dextrose could trigger the release of insulin which promotes movement of potassium into cells.
Potassium sparing drugs such as amiloride and spironolactone increase serum potassium by decreasing its renal excretion. Both are usually prescribed to prevent diuretic induced hypokalaemia when oral potassium is not tolerated. The recommended dose for amiloride is 5mg to 10mg twice daily, while the dose for spironolactone is 50mg to 100mg twice daily. Initial response to treatment should be reviewed every one to two weeks to avoid the risk of hyperkalaemia.
References:
- Beers M, Porter R, Jones T, Kaplan J, Berkwits M. The Merck manual of diagnosis and therapy. 18th ed. Whitehouse Station (NJ): Merck; 2006.
- Endocrinology Expert Group, Therapeutic Guidelines: Endocrinology. Version 4. Melbourne: Therapeutic Guidelines Limited; 2009.
- Mims Online [Internet]. St Leonards: UBM Medica; 2013 Apr. Available from: www.mimsonline.com.au/.
- Rossi S, editor. Australian Medicines Handbook 2013. Adelaide: Australian Medicines Handbook Pty Ltd; 2013.
- Wells B, DiPiro J, Schwinghammer T, Hamilton C. Pharmacotherapy handbook. 5th ed. New York: McGraw-Hill; 2003.
